The macular hole occurs most frequently in the elderly. Early detection and early treatment ensures better chances of gain in visual acuity.
1 – What is a macular hole?
A full thickness defect or discontinuity in the central part of the retina (also called fovea) is referred to as macular hole (figure 1). It’s a frequent cause of loss of central vision in the elderly.

Figure 1. Macular hole
2 – What are the causes of macular hole formation?
Predominantly it is idiopathic/ age-related or following blunt trauma to the eye.
3 – What is the mechanism of hole formation?
The most commonly encountered age-related type is caused by abnormal vitreoretinal adhesions which cause pulling of the fovea. This pulling of the fovea results in cyst formation which subsequently ruptures resulting in the formation of full thickness defect in fovea referred to as a macular hole.
4 – What are the symptoms of the macular hole?
Initially, patients complain of distortion of letters while reading and later on jumping of letters/splitting of letters. At later stages when the hole enlarges in size, patients complain of scotoma or the inability to see the area of interest when they focus on it. As the hole increases in size, there is a gradual decrease in visual acuity.
5 – What are the conditions associated with a macular hole?
Some patients have a macular hole coexisting with cataract in the same eye. It is always good to do a thorough retinal evaluation prior to cataract surgery to promptly diagnose conditions like these. Sometimes when cataract (opacification of lens) is significant which can make the diagnosis of macular difficult, it can be easily diagnosed with an OCT scan of the macula.
A few patients develop macular hole many years after successful cataract surgery causing a recent decrease in vision.
Sometimes patients delay in seeking attention to this problem thinking it could be to be the more common age-related eye condition called cataract which requires only an elective surgery.
6 – How is macular hole diagnosed?
OCT scan (a non-invasive imaging technique) of the macular area is done to confirm the diagnosis of the macular hole. It not only confirms the diagnosis but also measures the size of the macular hole and also analyses the layers of the retina including the photoreceptor layer. OCT is important to not only confirm the diagnosis but also to prognosticate regarding the visual recovery following surgery.
7 – What are the chances of visual recovery, post-treatment?
Two most important factors that determine the visual recovery after surgery for a macular hole are the duration of the hole as well as the size of the hole (figure 2). The smaller the hole and the lesser duration of onset of symptoms or decreased vision the better are the chances of visual recovery following surgery. The earlier the condition is diagnosed and earlier the patient is taken up for surgery the better are the chances of visual recovery.
It’s better to undergo surgery when the size of the hole is small and the vision loss is minimal than waiting for the hole to increase in size and the vision drastically reduced. Untreated macular hole does not result in complete blindness in the eye but the reading vision can be damaged permanently.

Figure 2. Stages of macular hole
8 – What is the treatment of a macular hole?
Surgery for macular hole involves vitrectomy (removing the vitreous gel from the inside of the eye), followed by internal limiting membrane peeling (internal limiting membrane refers to the thin acellular basement membrane lining the inner surface of the retina in contact with the vitreous). This is followed by fluid air exchange (removing of the fluid and infusing the air) and injection of a non-expansile concentration of special gases like SF6 or C3F8. Currently, for large holes, a technique of inverted ILM peeling is done and the ILM is stuffed into the hole. This technique vastly increases the success rate of closure of macular holes. The success rate of closure of macular holes is currently close to 95 % at Neoretina Eyecare Institute. Figure 3.

Figure 3. Intraoperative, through the microscope view of a macular hole surgery
9 – What post-operative care following macular hole surgery?
Following the macula hole surgery, most of the patients are advised to stay in a face-down position (figure 4.1) or prone position (figure 4.2) for the maximum possible time for 2 days. Face down position ensures that the gas bubble injected lies in apposition the hole and the surface tension effect of the gas bubble helps in sealing of the hole. Increasing the duration of the position ensures that strong adhesions formed and the hole stays closed.
Due to back pain or obesity if the patients are unable to maintain face down or prone position it is advisable to lie to one side. It’s strictly prohibited to lie supine position facing the ceiling in the immediate postoperative period.

Figure 4.1 Face down positioning

Figure 4.2 Prone positioning following macular hole surgery
10 – What is the best way to treat a cataract with macular hole?
For patients having a cataract as well as a macular hole it is recommended to perform a phacoemulsification and intraocular lens implantation surgery along with macular hole surgery
11 – What are the complications of macular hole surgery?
Complications of macular hole surgery include the development of cataract as well as the progression of cataract (which would require another surgery for its removal and intraocular lens implantation), development of retinal tears during surgery (which are treated with a laser during surgery) and lastly failure to close (chances of less than 5 %).
Case1. Macular hole, before surgery
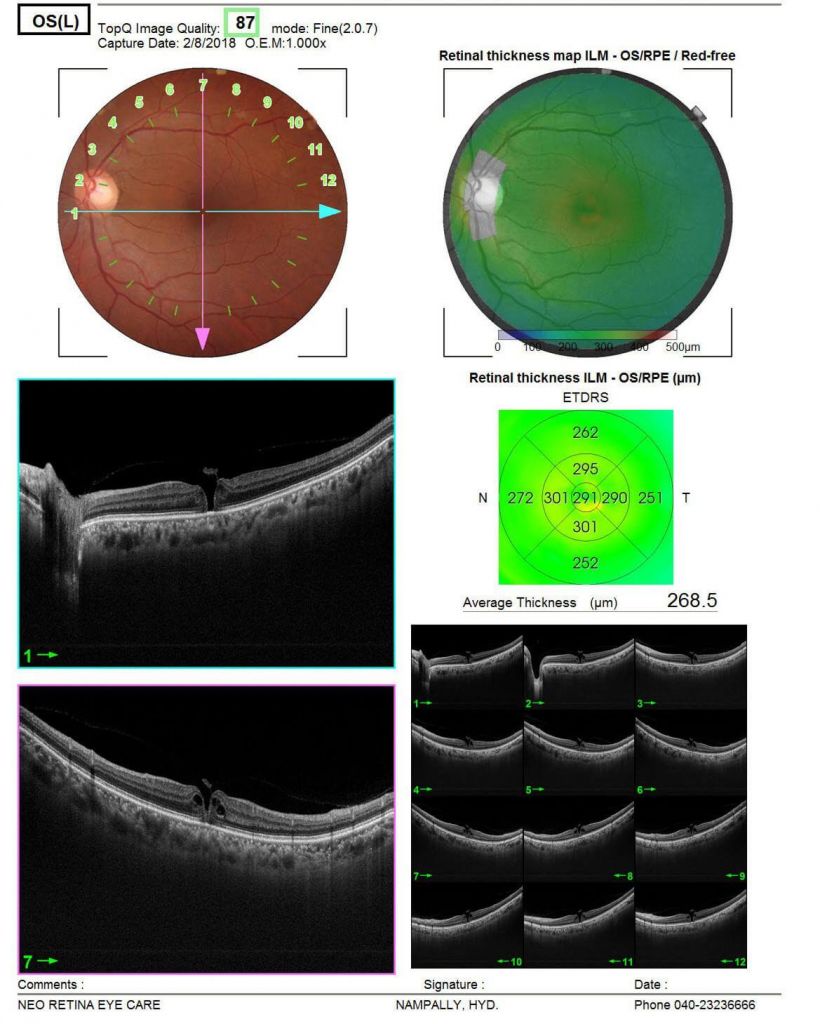
Case1: Closure after surgery
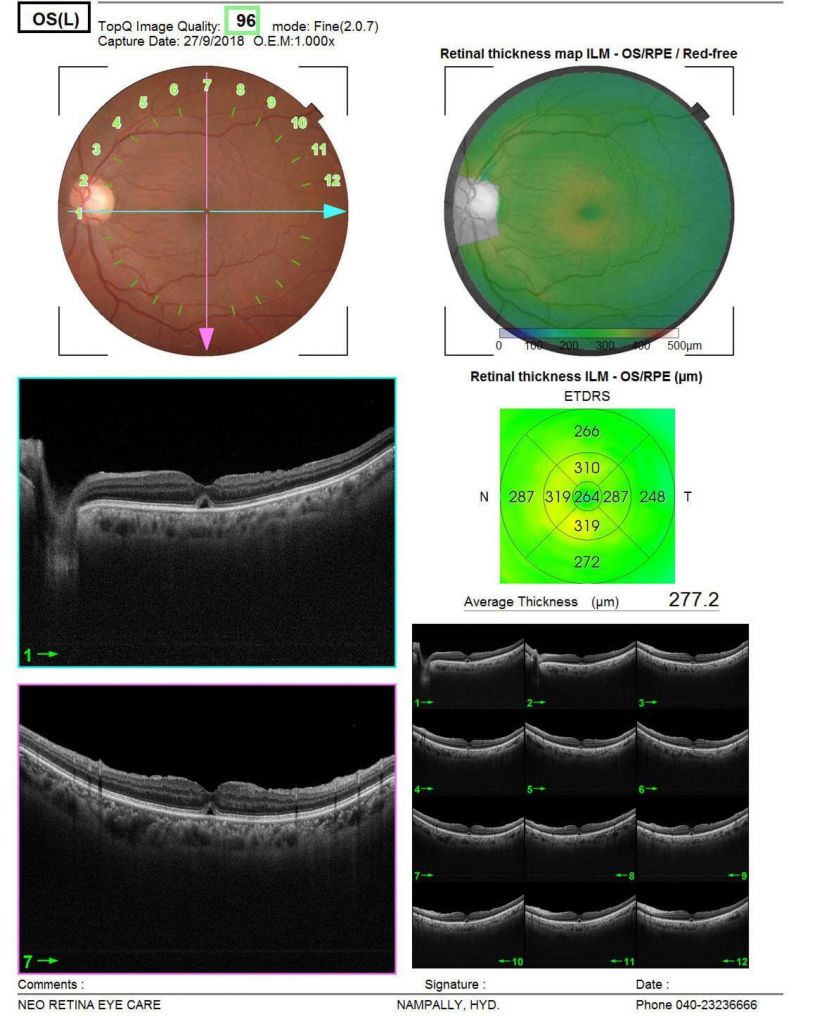
Case2. Macular hole before surgery
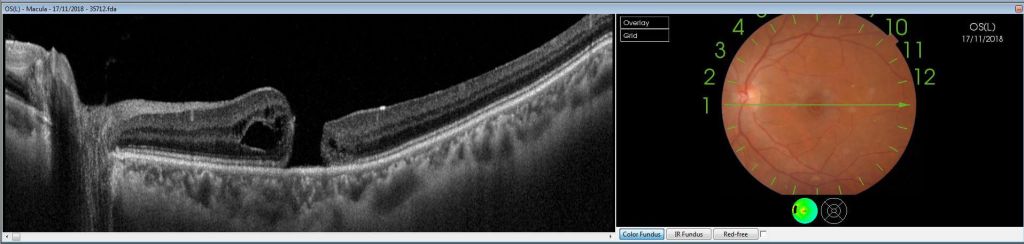
Case2. Closure after surgery
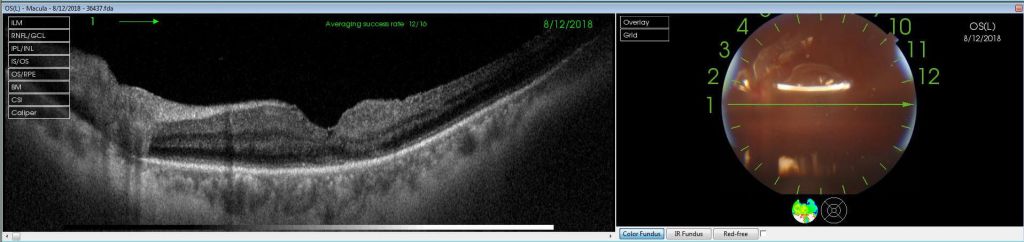
Case 3. Macular hole in a highly myopic patient, after and before surgery.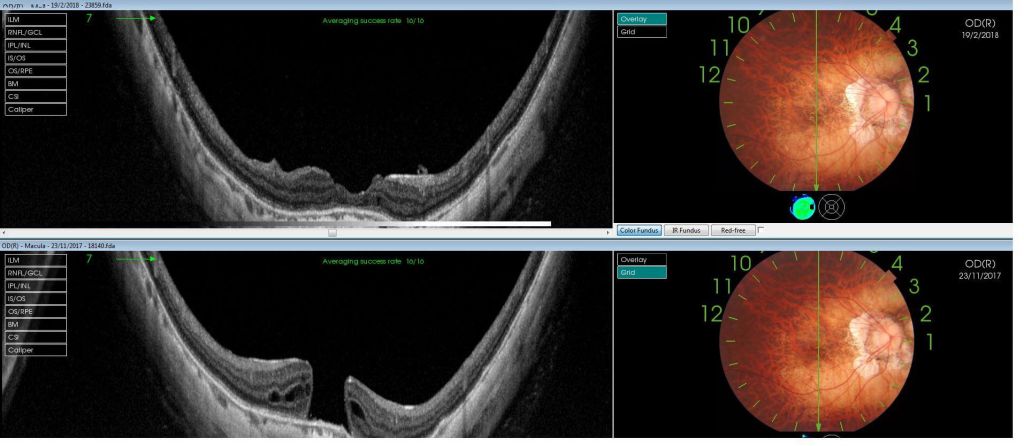
- Retinitis Pigmentosa Symptoms, Causes, and Treatment - September 23, 2019
- Diabetic Vitrectomy: A Quick Guide - June 7, 2019
- Macular Surgery: What You Should Know - June 5, 2019