Our Previous Blog Ocular Tuberculosis Part 3
Generally, tuberculosis is known to affect the pulmonary system, but in some cases, it can also affect other organs (extra-pulmonary) like eyes. Ocular tuberculosis or tuberculosis uveitis is a chronic infection caused by Mycobacterium tuberculosis. This infection can occur in or around the eye. It can occur with or without clinical evidence of pulmonary tuberculosis. In addition, it can affect any tissue of the eye, sometimes without any characteristic manifestation. Hence, establishing the diagnosis of ocular tuberculosis is a great challenge. However, prompt and accurate diagnosis and quick treatment can help save the patient’s vision.
What are the difficulties and what is the importance of an accurate diagnosis of ocular TB?
Ocular Tuberculosis is extremely challenging to diagnose for the following reasons:
- There is no uniform diagnostic criteria laid down
- Biopsy and molecular diagnosis from the eye lesions is a challenge because it is a paucibacillary (containing only few bacilli) disease.
- We still do not know whether it is a direct infection from bacteria or it is a hypersensitivity reaction to the bacterial antigen/protein.
- Eye TB has protean manifestations and it mimics many other diseases.
- There may or may not be any signs of systemic tuberculosis
However, getting the diagnosis right is very critical, especially in ocular tuberculosis because it has implications on treatment and final visual outcome for the patient. In the presence of an inaccurate diagnosis, inadvertent use of steroids or immunosuppressive agents, which are the most commonly used drugs for treatment of uveitis, may lead to reactivation of latent tuberculosis and can actually worsen the disease and prognosis for the patient. Moreover, an undetected active systemic TB may even be life-threatening if patient is treated with only steroids or systemic immunosuppression.
What are the diagnostic tests used for ocular TB?
Following is a brief description of the diagnostic tests we use and their rationale.
- Ocular Imaging: Depending on the primary site of involvement, following individual or combination of imaging techniques are used:
- External eye photography (Figure 1)
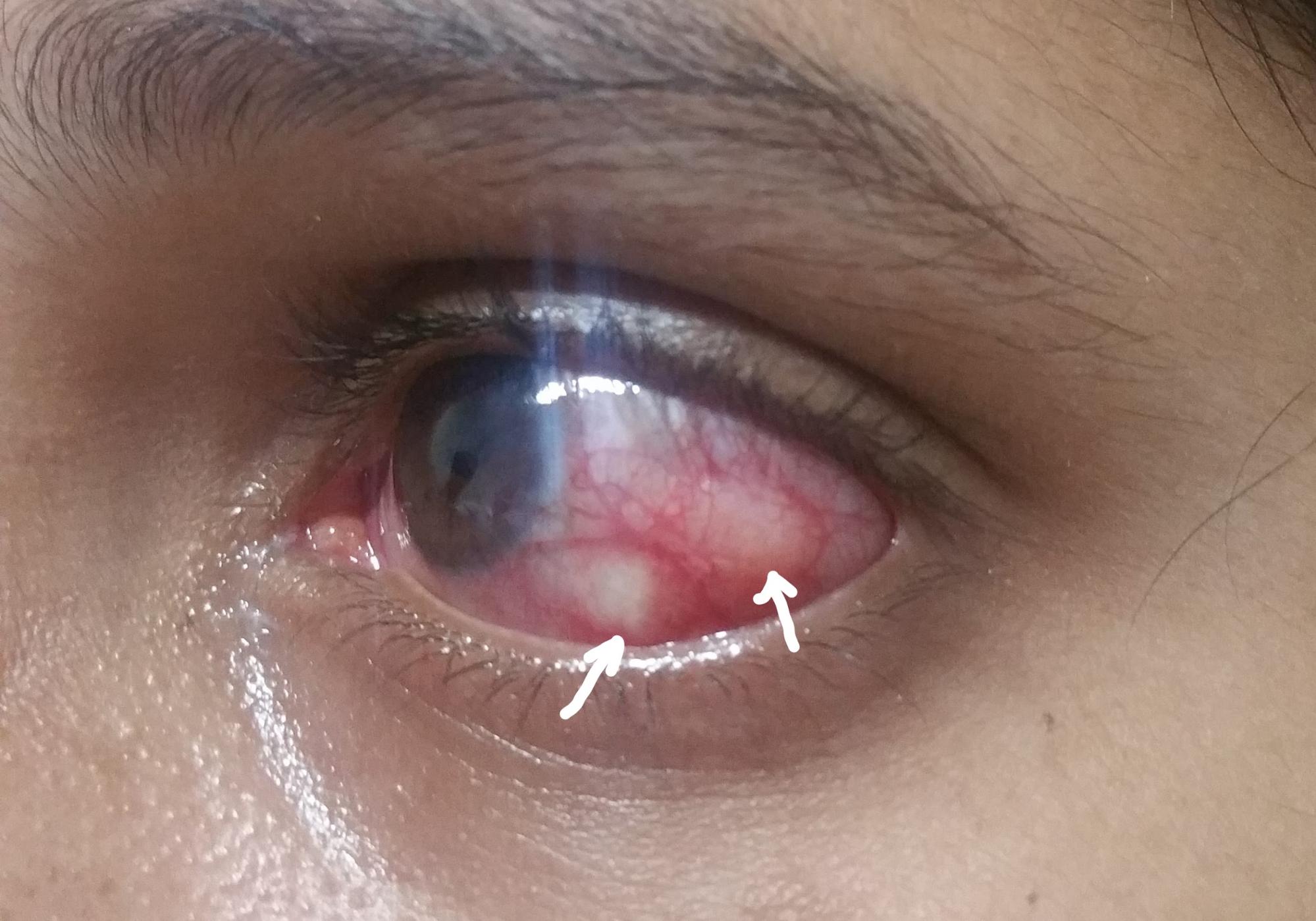
Figure 1. Left eye of a patient with multiple scleral nodules (arrows). - Fundus photography: a photograph of the retina (nerve layer at the back of the eye) (Figure 2)
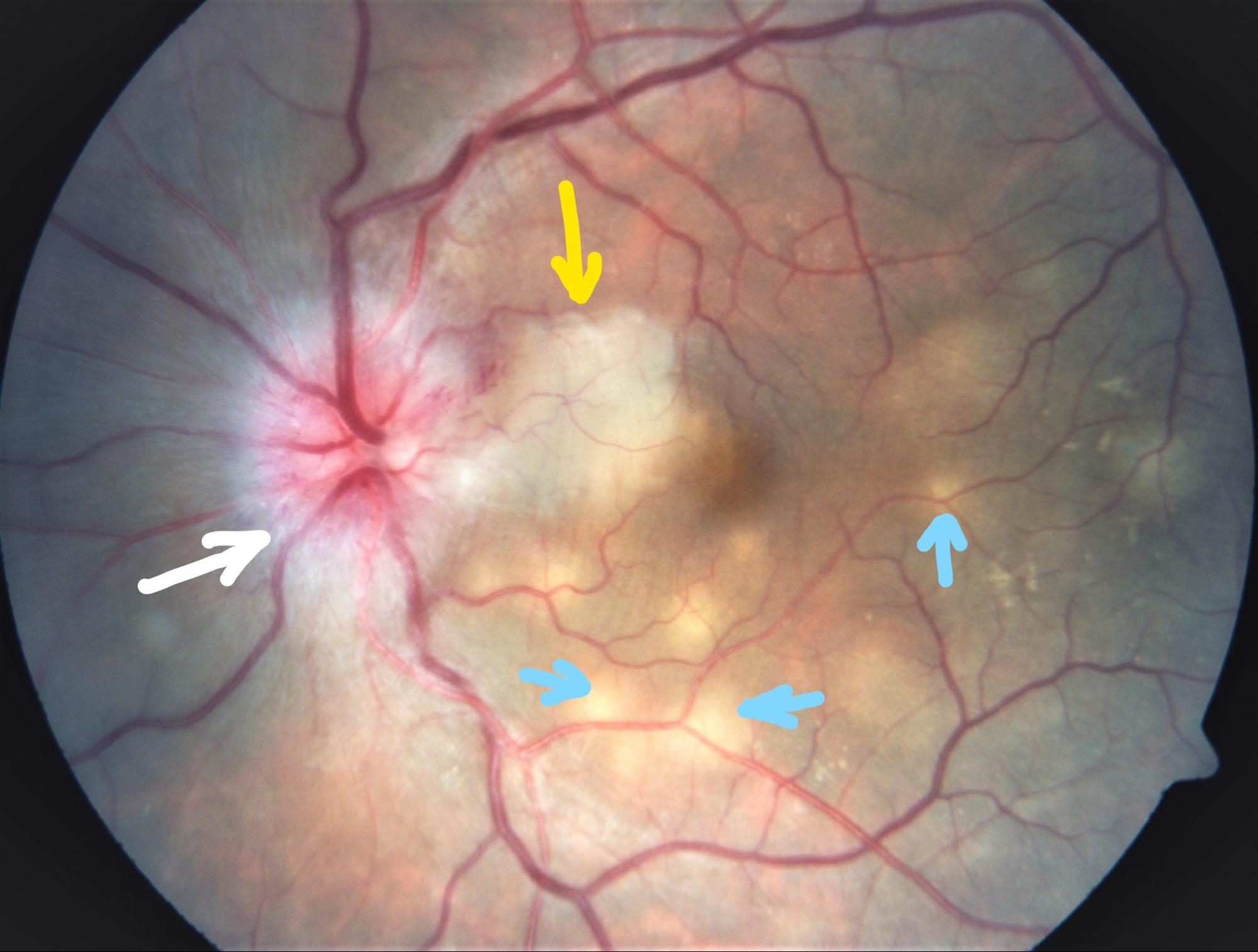
Figure 2. Fundus photograph of the left eye of a patient with optic disc swelling (white arrow) with whitening of adjacent retina (neuroretinitis, shown by yellow arrow)) and multiple deep yellow lesions (choroiditis, shown by blue arrows) - Fundus autofluorescence: photo of the retina using special filters where area of interest is the retinal pigment epithelium. (Figure 3).
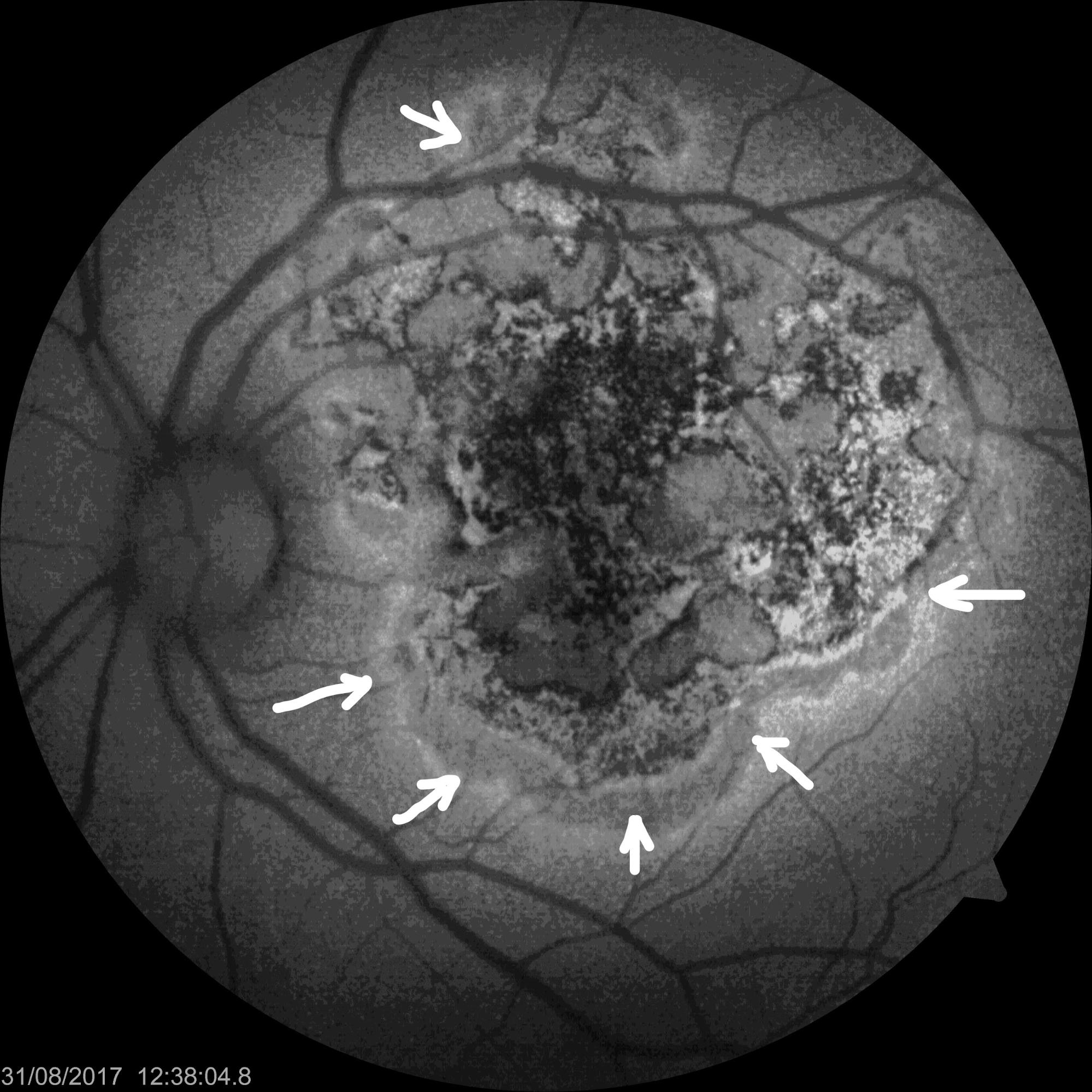
Figure 3. Fundus autofluorescence picture of a patient with left eye serpiginoid choroiditis (disease of the RPE and choroid, presumably due to tuberculosis). The lesions are active at the margins (arrows). - Fluorescein angiography: Where a fluorescein dye is injected in a vein of the forearm and its transit through the choroid, retina and retinal blood vessels is studied by photographs. (Figure 4)
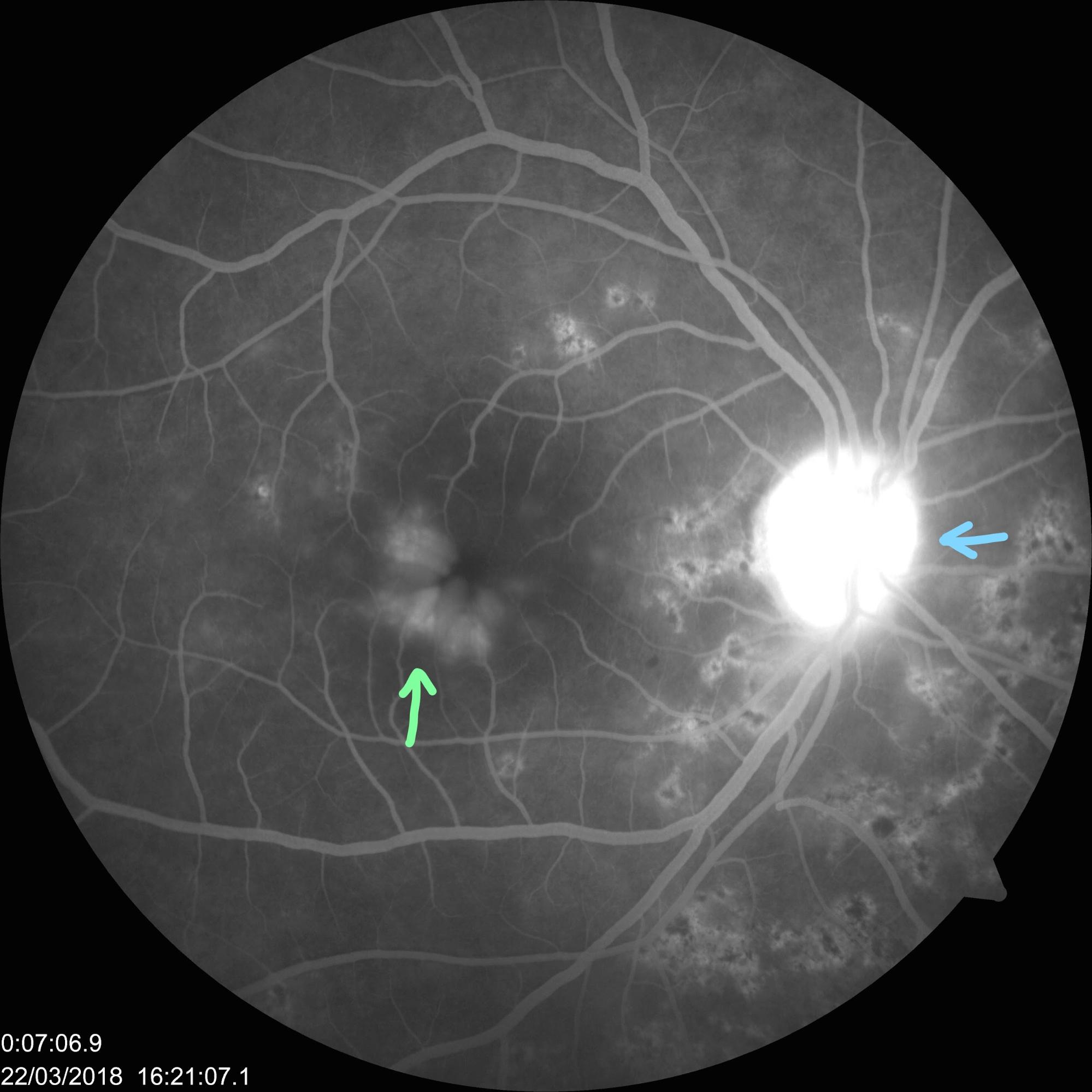
Figure 4. Fluorescein angiography picture of the right eye of a patient with posterior uveitis, showing a hot disc (bright signal at the optic nerve, shown by blue arrow)) and leakage at the macula (centre of the retina, shown by green arrow). - OCT: It is a non-invasive scanning method to study cross-section of the retina and choroid. It is particularly useful in studying the vitreo-retina interface, swelling/ fluid collection inside the retina (cystoid macular oedema) or under the retina (subretinal fluid), abnormality in various layers of the retina and choroid. (Figure 5)
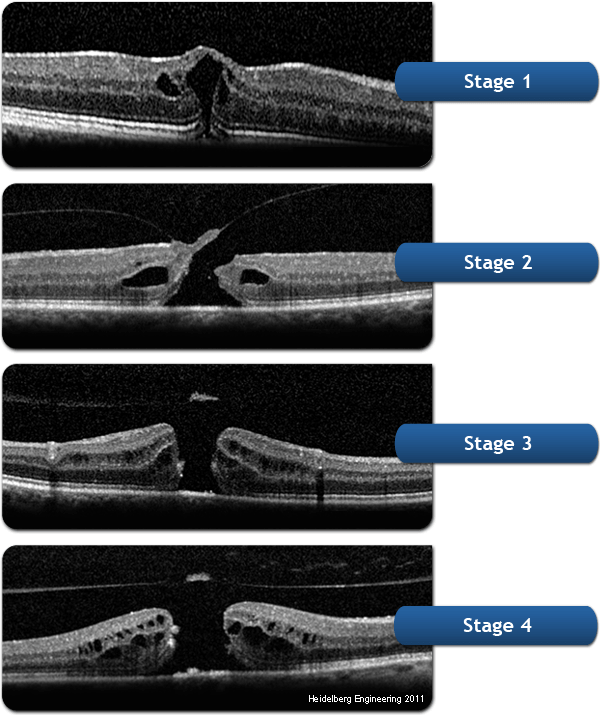
Figure 5. OCT picture of a patient with cystoid macular oedema (swelling of the centre of the retina), showing fluid spaces and the different layers of the retina. - OCT angiography: This is a non-invasive, no dye, no injection angiography to study the deep retinal and choroidal vasculature. (Figure 6)
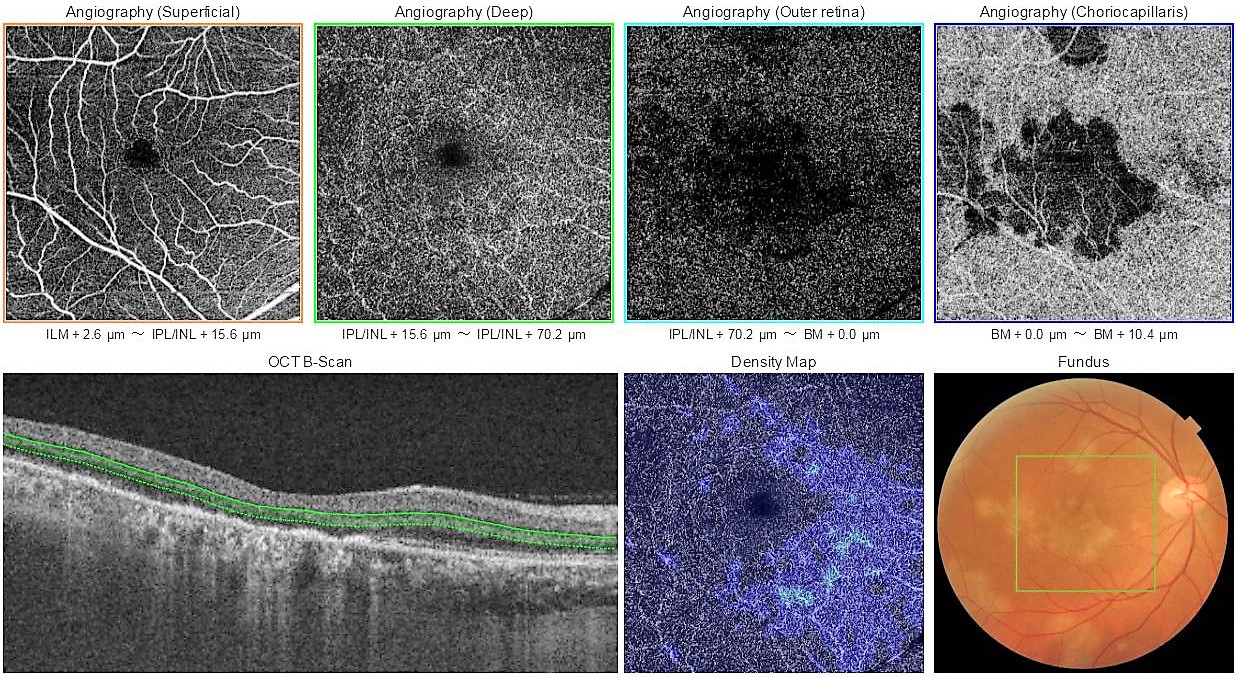
Figure 6. OCT angiography of the right eye of a patient with multifocal serpiginoid choroiditis, presumably due to TB, showing the vasculature (blood vessel network) in the deep retina and choroid. - B-Scan: This is a non-invasive scanning technique where a an ultrasound probe is placed on the closed eyelids of the patient. In uveitis, it is mainly used the study inflammation of the posterior sclera (white outer coat of the eye). (Figure 7).
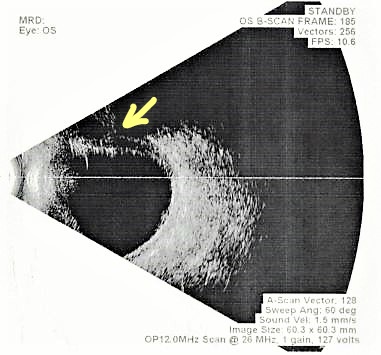
Figure 7. Ultrasound B-scan of a patient with scleritis (inflammation of the white portion of the eye) and superior exudative retinal detachment (arrow). - Ultrasound biomicroscopy (UBM): This is also a non-invasive scanning technique used mainly to study the anterior scleral lesions. (Figure 8).
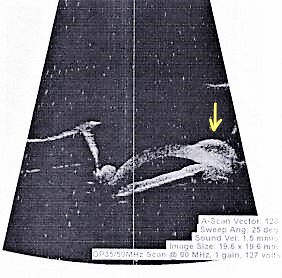
Figure 8. UBM scan of a patient with scleral abscess (arrow) due to tuberculosis - Visual fields: This is used to study optic nerve involvement due to disease or drug toxicity. (Figure 9)
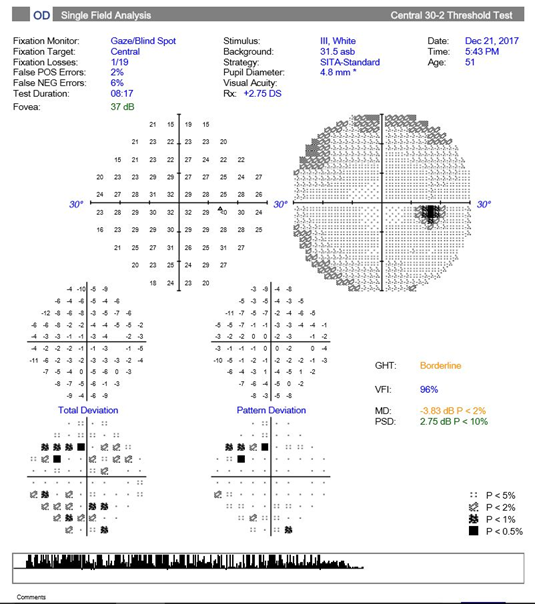
Figure 9. Visual fields report
- External eye photography (Figure 1)
Systemic investigation: We refer patients to an NABL accredited diagnostic laboratory for the following systemic tests:
- Mantoux test: It is a test of immunity to tuberculosis antigen. 0.1 ml 5 tuberculin units of purified protein derivative is injected into the skin of the forearm and reaction to it is measured after 48 hours. The test is considered positive (i.e. patient is likely to have latent / active tuberculosis) when the induration (skin swelling) is 10mm or more. At 10mm, the sensitivity (ability of the test to correctly identify those with the disease) of the test is 71% and specificity (ability of the test to correctly identify those without the disease) is 66%. In HIV positive patients >5 mm induration is considered a positive reaction. Mantoux test is cutaneous hypersensitivity to tuberculin antigen and it has been proven that cutaneous hypersensitivity correlates with ocular hypersensitivity. Thus this test is important in diagnosis of ocular disease.Sometimes, patients are told that a positive mantoux test has no meaning in our country because we all have taken BCG vaccination at birth. This does not hold true, as according to the recommendations of the Advisory Council for elimination of tuberculosis, Center for Disease Control and Prevention: Screening for tuberculosis infection in high-risk populations, the probability that the reaction in mantoux skin test is from the Mycobacterium tuberculosis antigen and not due to BCG increases:
- with increase in size of reaction,
- with a patient who has been in contact with a person who has TB,
- with family history of TB or patient’s country of origin has a high incidence or prevalence of TB, and
- with an increasing interval between vaccination and skin testing. Vaccination-induced reactions wane with time and are unlikely to persist for more than 10 years.
Also, even according the United States Preventive Services Task Force, any induration of more than 10 mm should not be attributed to prior BCG vaccination.
Recently, a new test, Quantiferon TB gold has been introduced for the detection of tuberculosis. This is a blood test that quantifies release of interferon gamma by stimulated sensitised T-cells in response to M. tuberculosis antigen ie. it measures release of a specific substance in the body in response to TB infection. Theoretically, it is not supposed to give false-positive results. However, about 41% healthcare workers and about 80.5% HIV positive patients with low-risk may show false-positive results. Like, Mantoux test it also does not differentiate between active and latent TB infection. According to the World Health Organization, “Latent Tuberculosis Infection: Updated and Consolidated Guidelines for Programmatic Management”, 2018, either a mantoux skin test or/ Quantiferon TB gold [interferon-gamma release assay (IGRA)] can be used to test for LTBI (strong recommendation, very low-quality evidence) and BCG vaccination should not be a determining factor in selecting a test. However, since there is no gold standard for testing for LTBI, we prefer, Mantoux test since it is cost effective and easily available.
- Mantoux test: It is a test of immunity to tuberculosis antigen. 0.1 ml 5 tuberculin units of purified protein derivative is injected into the skin of the forearm and reaction to it is measured after 48 hours. The test is considered positive (i.e. patient is likely to have latent / active tuberculosis) when the induration (skin swelling) is 10mm or more. At 10mm, the sensitivity (ability of the test to correctly identify those with the disease) of the test is 71% and specificity (ability of the test to correctly identify those without the disease) is 66%. In HIV positive patients >5 mm induration is considered a positive reaction. Mantoux test is cutaneous hypersensitivity to tuberculin antigen and it has been proven that cutaneous hypersensitivity correlates with ocular hypersensitivity. Thus this test is important in diagnosis of ocular disease.Sometimes, patients are told that a positive mantoux test has no meaning in our country because we all have taken BCG vaccination at birth. This does not hold true, as according to the recommendations of the Advisory Council for elimination of tuberculosis, Center for Disease Control and Prevention: Screening for tuberculosis infection in high-risk populations, the probability that the reaction in mantoux skin test is from the Mycobacterium tuberculosis antigen and not due to BCG increases:
Chest X-Ray / High-resolution Computed Tomography (HRCT) Chest:
Although traditionally chest X-ray is used for the diagnosis of pulmonary (lung) tuberculosis, it has been shown in a study published in 2014 in the International Journal of Infectious Diseases, that HRCT (high resolution CT scan of the lung) is better than chest X-ray in predicting lung TB, with a sensitivity of 96% versus 48%. A study published in the Turkish Thoracic Journal in 2016, supported the use of HRCT chest in the diagnosis of lung TB even in patients in whom the bacteria were not seen in the sputum test. In our study from Neoretina (Figure 10), we proved the utility of HRCT chest in the diagnosis of ocular tuberculosis even in patients who had a negative or inconclusive mantoux test. We concluded that HRCT has an important role in the accurate diagnosis of ocular tuberculosis, especially in the absence of other confirmatory tests. Correct diagnosis of this treatable condition is essential for the prevention of blindness from recurrent uveitis. This is also important to obviate the risk of reactivation of systemic tuberculosis from the use of steroid only therapy in this group of patients.
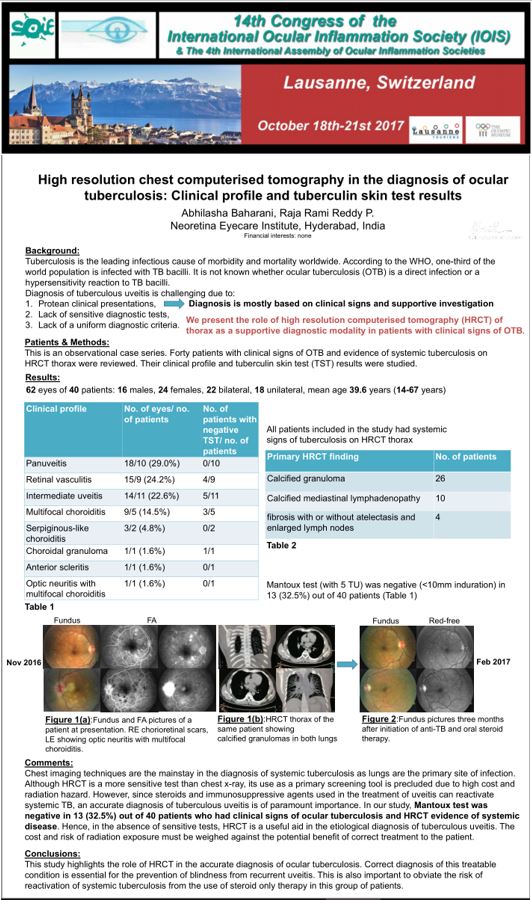
Figure 10. Our study presented at the Congress of the International Ocular inflammation Society, Lausanne, Switzerland, 2017.
What are the diagnostic categories of Ocular Tuberculosis?
At Neoretina, our treatment protocols are based on the latest Index-TB Guidelines, Guidelines on Extrapulmonary Tuberculosis in India, published by the Central TB Division, Ministry of Health and Family Welfare, Government of India in 2016. The following diagnostic categories have been defined:
- Possible ocular TB: Patients with the following (1, 2 and 3 together or 1 and 4) are diagnosed as having possible ocular TB:
- At least one clinical sign suggestive of ocular TB and other causes excluded.
- X-ray/CT chest not consistent with TB infection and no clinical evidence of extraocular TB
- At least one of the following:
i. Documented exposure to TB (family history of TB)
ii. Immunological evidence of TB infection (positive Mantoux or Quantiferon TB gold test) - Molecular evidence of Mycobacterium tuberculosis infection (confirmation through testing of fluid from the eye).
- Clinically diagnosed ocular TB: Patients with all the following (1, 2 and 3 together) are diagnosed as having probable ocular TB:
- At least one clinical sign suggestive of ocular TB, and other causes excluded
- Evidence of chest X-ray consistent with TB infection or clinical evidence of extraocular (outside the eye) TB or microbiological confirmation from sputum or extraocular sites
- Documented exposure to TB and/or immunological evidence of TB infection.
- Bacteriologically confirmed ocular TB: A patient with at least one clinical sign of ocular TB, along with microbiological (smear/culture) or histopathological confirmation of Mycobacterium tuberculosis bacteria from ocular fluids/tissues.
How is Ocular TB treated?
Patients in all the three described diagnostic categories are treated with anti-tubercular therapy (ATT) for at least 9 months. Longer duration of treatment is required for prevention of recurrences. During follow-up treatment is monitored by regular eye examination and eye scans, colour vision and liver function tests to look for any drug toxicity. Corticosteroids (local or systemic) and are used as adjunctive treatment for the control of inflammation. Locally steroids may be used as eyedrops, depot steroid near the outer coat of the eye (posterior subtenon injection) or as a low dose dexamethasone implant inside the eye (Ozurdex). We prefer local injections when the risk of systemic side effects of steroids are higher, like in pre-existing diabetes, hypertension (high BP), osteoporosis (weak bone structure) or when the disease is unilateral and systemic steroids use is not justified or when the patient is unable to tolerate systemic steroids.
How is response to treatment monitored?
Since microbiological confirmation might not be possible with ocular tissues, we monitor the response to treatment by the level of inflammation in the eye. Disease is said to be in remission when there is no inflammation for at least 3 months after completion of treatment. Relapse is when there is 2-step increase in inflammation after complete remission. Treatment failure is when there is no decrease in inflammation or less than 2-step decrease in inflammation after 3 months of ATT. In case of treatment failure, we look to rule out other causes of uveitis. Sometimes a paradoxical reaction (increase in inflammation to tuberculosis antigen) may occur, generally 2 months after starting ATT. In such cases steroid therapy needs to be stepped up. Lastly, we take fluid from the eye for molecular diagnosis of tuberculosis and to test for drug resistance.
Is surgery also required for the treatment of Ocular TB?
Surgery may also be required, usually when there are complications of uveitis such as:
- Neovascularization (growth of abnormal blood vessels in the retina which tend to bleed) in cases of retinal vasculitis (inflammation of retinal blood vessels). Such cases may be treated with retinal laser, which is an outpatient procedure. In case of non-resolving vitreous haemorrhage (bleeding inside the eye), a vitrectomy surgery (removal of the vitreous, the gel occupying the inside of the eye, where the bleeding has occurred) may be required.
- Persistent floaters after completion of treatment. In such cases also vitrectomy may help.
- Cataract: cataract surgery with intraocular lens implantation is done.
- Glaucoma: If medically uncontrolled, surgery may be required to control the intraocular pressure.
In summary, diagnosis of ocular tuberculosis is a difficult task but a keen clinical eye and a combination of diagnostic tools and methods help in the same. It is important for patients and clinicians to understand the diagnostic and treatment methods in order to remove the stigma and fear associated with this disease. Like in every other branch of medicine, an early, accurate diagnosis, and prompt and appropriate treatment is so critical in achieving favourable results. A systematic approach and proper diagnosis at the initial stages, before complications of the disease set in, helps to avoid inadvertent use of steroids with recurrence of tuberculosis uveitis and improves visual outcome of this sight-threatening disease several fold.
- A Simple Guide to Complicated Cataract Causesand Treatment - June 11, 2019
- Choosing the Right Intraocular Lens: Make an Informed Decision - February 28, 2019
- Intravitreal Injections: Indications, Procedure, Do’s, Don’ts and Myths - February 13, 2019