Our Previous Blog Ocular Tuberculosis Part 2
How common is tuberculosis? The magnitude of the problem.
Tuberculosis is one of the most widely prevalent diseases in the world. However, it’s prevalence is quite underestimated. In 2015, WHO had called it a global emergency being the most common single cause of morbidity and mortality in the world, causing 3 million deaths per year. India tops the list of 22 countries identified as contributing 80% of the world’s total burden of TB. One-third of the world population is infected with TB bacilli, out of which only 10% are symptomatic i.e. only 10% have fever, night sweats, cough and weight loss, rest 90% are asymptomatic and have latent TB infection (LTBI). An estimated 5% of persons with LTBI (100 million population) will progress to active TB disease in the future.
What is extrapulmonary TB?
Out of all the cases of tuberculosis, 20% are extrapulmonary, i.e. affect organs other than the lungs. After Mycobacterium tuberculosis bacilli has been inhaled, the organisms undergo phagocytosis (ingestion) by alveolar macrophages (cells comprising the defense mechanisms of the lung), resulting in bacterial containment. In some patients, the bacilli may disseminate systemically, establishing latent infection at extrapulmonary (outside the lungs) sites, with the potential to reactivate at a later time. Reactivation of latent TB usually occurs when the host’s immune system is compromised. Extrapulmonary TB is believed to result from reactivation of latent mycobacteria residing within resident reticuloendothelial cells.
About 60 % of these cases of extra-pulmonary TB have no evidence of pulmonary TB. This means that a person with ocular TB may have no evidence of lung disease. The prevalence of ocular TB is reported as 1-4% in low endemic areas but it rises to 10-26% in high endemic countries like India.
How does TB infection reach the lung? -Pathogenesis.
When a person with TB infection coughs or sneezes droplets containing mycobacteria are released in the environment. These droplets are about 200 microns in size and remain suspended in the air for about an hour.

Figure 1. Diagrammatic representation of pathogenesis of tuberculosis. Derived from graphics in Nature Reviews, Microbiology.
The diagrammatic explanation (Figure 1) can be followed below.
1. Bacterial entry: The infected droplets suspended in the air are inhaled by another person and bacteria enter their system. The inhaled bacteria generally settle in the upper respiratory tract (the nose and the throat) where they do not survive for long. Some smaller particles might find their way into the lungs and their alveoli (air sacs of the lungs which are responsible for exchange of oxygen and carbon dioxide between the lungs and the bloodstream). It is here that the infection occurs.
2. Bacterial multiplication: Alveolar macrophages (a group of white blood cells found in tissues) engulf the bacteria. Mycobacteria are unique in that they do not allow fusion of phagosome with lysosome, ie. there are mechanisms by which they prevent themselves from being killed inside the macrophages. The bacteria, in fact, multiply in these unactivated macrophages until the macrophages burst. Mycobacterium tuberculosis bacteria continue their slow replication (multiplying once in 24 hours), taking about one month to form a colony.
3. Cell mediated immunity: Dendritic cells which are an important component of our immune system are found in tissues where our body comes in contact with the external environment, namely skin and lung alveoli. These dendritic cells identify foreign substances or bacteria entering the body and engulf them. They then break these foreign substances into smaller particles. These smaller particles (potential antigens) are transported to lymph nodes (bean shaped structures in the body that contain white blood cells which fight against bacteria and diseases) where they’re are presented to T cells (a component group of white blood cells). If the T cells have receptors for the presented antigens, the get activated and release inflammatory molecules like interferons and tumour necrosis factor. These inflammatory cytokines activate other T cells and macrophages. Thus cell mediated immunity is activated. This takes about 48-72 hours and hence known as delayed hypersensitivity.
4. Tubercle/ Granuloma Formation: The T-cells now return to the site of infection and result in granuloma (tubercle formation). A granuloma consists of centrally placed infected macrophages, surrounded by foamy macrophages (known so for their foamy appearance caused by ingestion of LDL cholesterol), which are further encircled by a ring of T-cells, all contained in a fibrous capsule. Bacteria contained inside a tubercle/granuloma is known as latent TB infection (LTBI).
Sometimes, like in children or persons with severely suppressed immune systems, the body may not be able to contain and isolate the bacteria inside tubercles. In such cases, primary progressive tuberculosis results.
Tubercle/granuloma formation does not result in permanent containment of infection. When the immune system weakens, the outer fibrous ring of the tubercle breaks down releasing the TB bacteria and causing reactivation of infection. This results in secondary progressive tuberculosis. 3-5% of immunocompetent individuals with LTBI may suffer reactivation in 2 years and a further 3-5% develop reactivation beyond 2 years.
5. Cavitation: Infected macrophages in the centre of the granuloma may get damaged and liquefy. This liquid provides a good medium for the bacteria to multiply outside the macrophages. As the bacteria multiply, the tubercle enlarges and may rupture into adjacent lung tissue resulting in cavity formation. This is also a form of secondary progressive tuberculosis. Wherever these newly released bacteria reach in the body, again the process of T cell activation and tubercle formation occurs, as described earlier.
How do TB bacteria reach the eye and where do they localise? -Pathology.
Once secondary progressive tuberculosis occurs, the released bacteria can lodge anywhere in the body including the eye. Inside the eye, studies have confirmed, that although retina and uvea get affected with tuberculosis, the Mycobacteria are preferentially localised to the retinal pigment epithelium (Figure 2). The retinal pigment epithelium (RPE) is the pigment layer of the retina, just behind the neurosensory retina. It provides nourishment to the retinal visual cells and is firmly attached to the underlying choroid (uvea) and overlying retinal visual cells. The reason for this preferential localisation of mycobacteria in the RPE is that the RPE shares quite a few features with alveolar macrophages which help the survival of mycobacteria. Like alveloar macrophages, RPE also expresses complement and toll like receptors which are important for mycobacterial recognition and phagocytosis (ingestion) (Figure 3). Moreover, like in alveolar macrophages, mycobacteria can evade destructive mechanisms in the RPE and thrive inside them without killing the RPE cells. Thus mycobacteria are sequestered in the viable RPE cells and can survive inside them for long periods of time. This is why ocular tuberculosis/ tuberculosis uveitis tends to be a recurrent disease with a normal appearing RPE and a longer course of anti-TB therapy is required in these cases to completely eliminate the infection.
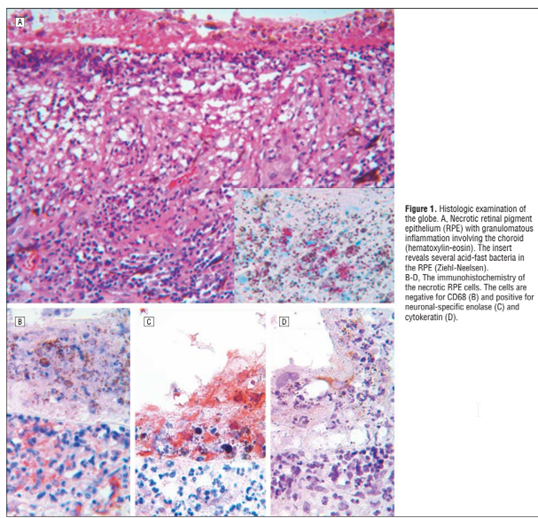
Figure 2. Necrotic RPE with granulomatous inflammation. Inset shows several acid fast bacilli (TB bacteria) in the RPE. Derived from: Rao, N.A., Saraswathy, S. and Smith, R.E., 2006. Tuberculous uveitis: distribution of Mycobacterium tuberculosis in the retinal pigment epithelium. Archives of Ophthalmology, 124(12), pp.1777-1779
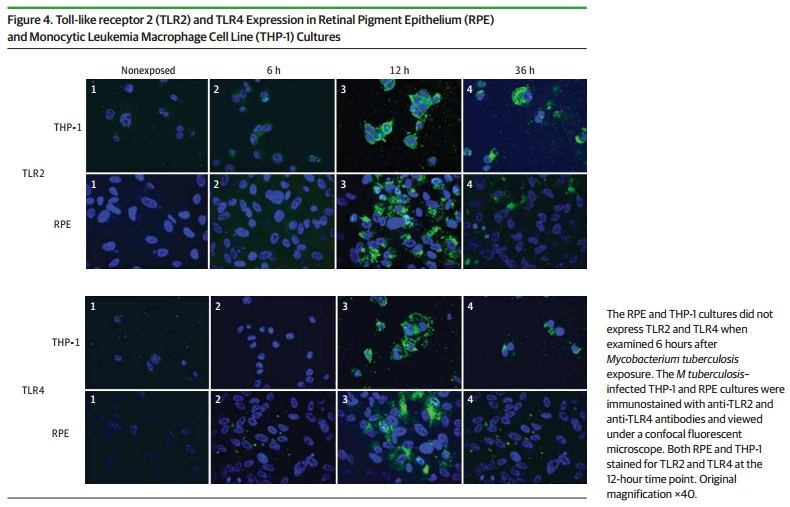
Figure 3. Immunostained picture of RPE and macrophage cultures, showing expression of toll-like receptors (TLR-2 and TLR-4, important for recognition of mycobacteria) at 12 hours. Nazari, H., Karakousis, P.C. and Rao, N.A., 2014. Replication of Mycobacterium tuberculosis in retinal pigment epithelium. JAMA ophthalmology, 132(6), pp.724-729.
To summarise, it is important for clinicians and patients to be aware of the magnitude of tuberculosis, which is a global emergency with an increasing prevalence, especially in the post HIV era. An understanding of the pathogenesis of TB in the lung and in the eye helps clinicians and patients understand the disease manifestations, treatment rationale and why adherence to treatment is so important not only for individual benefit but also to reduce the global burden of disease.
To continue reading on this subject, visit our next blog Ocular Tuberculosis Part 4
- A Simple Guide to Complicated Cataract Causesand Treatment - June 11, 2019
- Choosing the Right Intraocular Lens: Make an Informed Decision - February 28, 2019
- Intravitreal Injections: Indications, Procedure, Do’s, Don’ts and Myths - February 13, 2019