A cataract is clouding of the natural crystalline lens of the eye. This obstructs the passage of light onto the retina at the back of the eye and affects the person’s ability to see clearly. Generally, cataract is seen in old age and such type of cataract is known as a senile cataract. If left untreated cataract leads to blindness.
What is complicated cataract?
A complicated cataract is opacification of the natural lens of the eye due to inflammatory conditions of the eye or uveitis. This includes anterior uveitis, intermediate uveitis or posterior uveitis. Cataract formation in retinitis pigmentosa, retinal detachment or secondary to glaucoma is also often called a complicated cataract.
What is the difference between a complicated cataract and a senile cataract?
As discussed, complicated cataract develops secondary to uveitis and hence it can affect people of any age, including children who are affected with uveitis, whereas senile cataract affects only the elderly.
Senile cataract is generally nuclear (involving the central core of the lens) whereas complicated cataract generally first affects the posterior axial cortical fibres and is known as a posterior subcapsular cataract.
In senile cataract vision is lost gradually with an initial reduction in contrast sensitivity whereas blurring of vision is more dramatic and rapid in complicated cataract as it affects the visually important posterior central part of the lens, causing significant scattering of light passing through it.

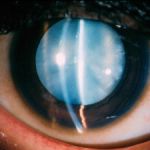
Nuclear senile cataract
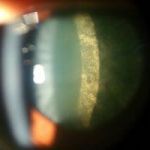

Types of complicated cataract
How to prevent complicated cataract?
A complicated cataract is especially disabling in young patients for 2 reasons: the cataract itself hampers vision and after cataract surgery, the non-accommodating monofocal intraocular lens makes near vision difficult without glasses. Early consultation with a Uveitis Specialist may help prevent the development of complicated cataract and reduce its severity as to obviate the need for cataract surgery. If Uveitis is treated in time with good control of inflammation and steroids are used only for initial management and control of inflammation is maintained with non-steroidal immunosuppressant therapy, the complicated cataract may be prevented to an extent or not be severe enough to require surgery. It is also important to know that steroid therapy for uveitis may itself cause cataract or lead to its progression. Patients must be warned against self-medication with steroid eyedrops as very often Uveitis may even be treated without the use of steroids. Hence, patients who self medicate only inflict upon themselves more problems (such as cataract and glaucoma), than the disease itself. Medication for uveitis must be started and stopped only according to an Uveitis expert’s advice and never on your own.
Treatment Options Available for Complicated Cataract
Cataract surgery is the most effective treatment for complicated cataract, but the decision and timing of surgery depend on the following factors:
- Degree of inflammation. Results of surgery are good when inflammation is under control.
- Surgery may be hastened if cataract obscures the view of the retina which in turn impacts treatment decisions.
- Impact of the cataract on vision. If the cataract is not disabling enough and vision can be adequately corrected with glasses, cataract surgery may be deferred.
Why is complicated cataract surgery special?
Complicated cataracts are often accompanied by other problems such as posterior synechiae (adhesions between iris and lens), anterior synechiae (adhesions between iris and cornea) and glaucoma (increased intraocular pressure) which have to be tackled simultaneously along with the cataract.
“Routinel” cataract surgery is done under topical anaesthesia and takes about 10 minutes. Complicated cataract surgery generally may require local anaesthesia and takes longer as additional procedures may be required. If posterior synechiae is present it has to be released before cataract surgery can be performed. If the pupil does not dilate because of posterior synechiae, pupil expanders or iris hooks need to be used.
During surgery, the clouded lens or cataract is removed by phacoemulsification and replaced with a clear artificial lens. The intraocular lens, i.e. the artificial lens, is positioned in the same place as the natural lens and becomes a permanent part of the eye.
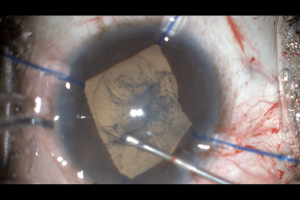
Complicated cataract surgery in progress with the help of iris hooks
What to expect after complicated cataract surgery?
Neoretina is adept at dealing with all kinds of cataracts and surgeons are experts at microincision cataract surgery with very good results and quick recovery. After routine senile cataract surgery, patients can expect a clear vision on day 1, but after complicated cataract surgery, visual recovery depends on the following factors:
- Status of the retina: patients with untreated or inadequately treated uveitis or those who present late may develop a scar on the macula (the central most important part of the retina which is responsible for accurate vision). In such cases whatever vision is lost due to the cataract is regained but final vision will depend on the status of the retina.
- Status of the optic nerve: Many a time the optic nerve may be damaged due to uveitis itself or due to glaucoma. In such cases also, final vision depends not only on the cataract but also on the status of the optic nerve. Your doctor will let you know the prognosis beforehand.
Uveitis is a systemic disease and requires prolonged treatment with systemic medication. Hence, after cataract surgery, patients should never assume that uveitis treatment is over and they can discontinue their medication. Medication has to be continued according to the doctor’s advice. Also, unlike routine cataract surgery, patients who undergo surgery for complicated cataracts may require more aggressive and prolonged topical steroid therapy, ie more frequent and longer use of postoperative eyedrops than the “routine” cases.
The Exclusive Uvea Department at Neoretina is adept at treating all kinds of Uveitis, infectious and non-infectious, and initiation and safe maintenance of non-steroidal systemic immunosuppressive therapy. This helps inadequate control of inflammation and excellent results following cataract surgery with very high success rates.
- A Simple Guide to Complicated Cataract Causesand Treatment - June 11, 2019
- Choosing the Right Intraocular Lens: Make an Informed Decision - February 28, 2019
- Intravitreal Injections: Indications, Procedure, Do’s, Don’ts and Myths - February 13, 2019