Vitrectomy refers to a surgical procedure which involves removal of the vitreous gel from the eye. It is a surgical procedure where small ports are created to introduce instruments into the eye and then the surgery performed with the aid of a vitrectomy machine which delivers high speed cutting to the cutting probe and a light source for visualisation of the inside of the eye and also requires high end microscope fitted with special lens system which gives a wide angle view of the entire retina.
Traditionally the surgery was performed using a 20 gauge instrument which needed the opening up of conjunctiva and then designing a 1.4 mm incision on the eye.
With rapid development in the instrumentation, smaller gauge instruments like 23 gauge, 25 gauge, and 27 gauge are being used in order to minimize the trauma to the eye. Smaller gauge instruments also help in working very close to the retina with a greater degree of safety. Moreover, the surgery with smaller gauge instruments is sutureless. This results in quicker surgeries, lesser postoperative inflammation, tissue scarring and more rapid healing of the wound. The advent of high-speed cutters (5000 cuts per minute) has also resulted in greater precision in surgeries with features which improve the safety of the surgical procedure thereby increasing the quality of surgeries. At Neoretina, we perform sutureless Microincision vitrectomy surgeries (MIVS).
Vitrectomy is sometimes accompanied by procedures like scleral buckle placement in case of retinal detachment or trauma. Similarly, procedures like membrane peeling and LASER are adjuvant steps in vitrectomy. Air, gas, Silicone oil or heavy liquids may also be used during the surgery. Air or gas spontaneously gets absorbed in a few days after the procedure. It is advisable to avoid flights or travel to high altitude areas until the gas has been completely absorbed. Silicone oil when placed will need another surgery 3- 6 months after the injection for their removal. When oil or gas are placed inside the eye after vitrectomy, postoperative positioning usually in the prone position needs to be maintained for best results.
What is a diabetic vitrectomy?
Diabetic vitrectomy refers to vitrectomy surgery performed for advanced stages of diabetic retinopathy for which other treatments like laser photocoagulation and intravitreal injections would not be of any help.
Diabetic vitrectomy refers to surgeries done for tractional retinal detachment, vitreous hemorrhage, subhyaloid hemorrhage, which are all complicated endstage proliferative diabetic retinopathy presentation. Diabetic vitrectomy is also offered for vitreomacular traction and chronic diabetic macular edema which is resistant to treatment with intravitreal injections.
How is diabetic vitrectomy different for vitrectomy done for other indications?
Diabetic vitrectomy is some of the most complex eye surgeries as they are done in advanced stages of diabetic retinopathy where the entire retina is diseased and has signs of ischemia (loss of blood supply). They also have membranes on the retina which are multiple pegs with varying degree of strength to the underlying retina. Complete removal of these membranes without any damage to the underlying retina and without causing any retinal tear or major bleeding happening is a tough challenge always. These surgeries test the patience and character of the operating surgeon. They always have to approach with a lot of patience and an unhurried approach. Young or inexperienced vitreoretinal surgeons typically are skeptical about operating on these cases.
Visual recovery after a diabetic vitrectomy depends on the duration of retinal detachment and vitreous hemorrhage, therefore, earlier operated the better. Visual recovery depends on the blood supply of the macula the central part of the retina. Ischaemia (loss of blood supply) of the macula carry a poor visual prognosis. Optic nerve status also determines the visual recovery. The healthy optic nerve carries a good visual prognosis and vice versa.
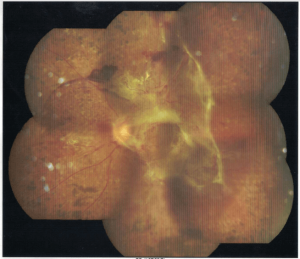
Diabetic retinopathy with tractional retinal detachment
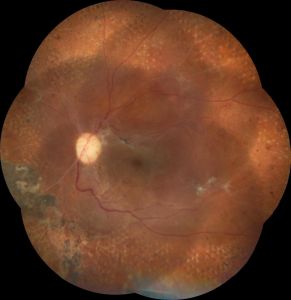
Same patient after diabetic vitrectomy
Preoperative investigations
Careful examination and documentation of findings including undilated slit lamp evaluation to look for new vessels on iris (NVI) and gonioscopy to look for angle new vessels (NVA). Both NVI and NVA carry a poor visual prognosis.
One would also see if there is any coexisting cataract which may also need to be addressed (cataract removal with IOL implantation ) in the same session.
Patients are expected to ensure diabetes and other diseases like hypertension and ischaemic heart disease are adequately controlled before embarking on vitrectomy surgery. It’s preferable to consult a physician and involve him in the decision to undergo vitrectomy surgery. In patients who are taking blood thinners like aspirin and clopidogrel are advised to stop these medications 3 days prior to surgery to decrease the chances of bleeding which is a common complication that we encounter during surgery.
Most of the surgeries are performed as outpatient/ daycare. Patients at neoretina are expected to be admitted at 7 30 am in the morning after taking breakfast and all other medication. They are typically discharged at 4 pm, a few hours after surgery. The surgeons at Neoretina provide all useful information to the patient as to what to expect after surgery, head positioning, use of the eye patch, medications, drops, and other general activities.

Microincision sutureless diabetic vitrectomy in progress
- Retinitis Pigmentosa Symptoms, Causes, and Treatment - September 23, 2019
- Diabetic Vitrectomy: A Quick Guide - June 7, 2019
- Macular Surgery: What You Should Know - June 5, 2019