Keratoconus (kerato: Cornea; konos: Cone) is a Greek word. It is a multifactorial non-inflammatory, progressive disease with biomechanical, biochemical, genetic, and environmental pathophysiology. Keratoconus is characterized by a steepening and thinning of the central and paracentral cornea causing myopia and irregular astigmatism. This eye disease affects approximately 1/2000 people of all races and both sexes equally. The onset of this disease is during the second decade of life around puberty. Keratoconus is bilateral and asymmetric ectatic eye condition which progresses until life’s fourth decade.
Screening and Diagnosis of Keratoconus
Diagnosis of keratoconus is really challenging. Your ophthalmologist will have to conduct detailed eye examination and review your family and medical history. You will have to undergo various eye tests to determine details about the cornea shape. Some common screening tests to diagnose keratoconus include:
- Eye refraction: With the help of special tools and equipment, your ophthalmologist will check for eye and vision problems. You may be asked to look through phoropter (a device that contains wheels of several lenses). This helps to judge the best combination that offers the sharpest vision. Some eye doctors use a retinoscope to evaluate the eyes.
- Slit-lamp examination: A vertical beam of light is directed on the surface of your eye in this test to view the eye. With a low-powered microscope, your doctor will evaluate the shape of the eye cornea and check for any other potential eye problems.
- Keratometry: In this test, your ophthalmologist will focus a circle of light on the eye cornea and measure the reflection. This test helps to determine the basic shape of the cornea.
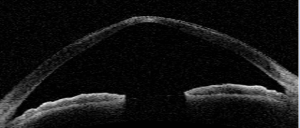
- Computerized corneal mapping: Your eye doctor will carry out special photographic tests, like corneal topography and optical coherence tomography. These tests record thickness and take cornea images to create a detailed map of your cornea shape and surface.
Keratoconus Treatment
Depending on the severity of the eye condition and its progression, treatment varies. For mild to moderate keratoconus use of eyeglasses or contact lenses can help. For the majority of people, the shape of the cornea becomes stable after some years and do not cause severe vision problems or need further treatment.
In the early stage of Keratoconus, eyeglasses or soft contact lenses help to correct blurry or distorted vision. But some patients frequently need to change their prescription for contact lenses or eyeglasses as their shape of corneas change. Next step in the treatment is hard contact lenses that are made to fit the cornea. In case the rigid lenses are not comfortable, your ophthalmologist may recommend ‘piggyback lenses’, hybrid lenses or scleral lenses. However, in some people, the cornea becomes extremely thin or the patients find it difficult to wear contact lenses, which call for corneal surgery.
Other Therapies
Corneal cross-linking: In this treatment, the cornea is saturated with riboflavin drops and then treated with ultraviolet light. This procedure leads to a chemical reaction to strengthen the collagen protein in the cornea, thereby helping to stabilize the cornea and minimize the risk of progressive vision loss early in the disease.
Surgery: Patients with corneal scarring, poor vision with the prescription lenses; an inability to wear contact lenses or extreme thinning of the cornea needs surgery. Depending on the severity of Keratoconus and the location of the bulging cone, your ophthalmologist will suggest the best type of surgery.
Surgical options for treating Keratoconus include:
Corneal inserts: In this type of surgery, your eye surgeon will place clear, tiny, crescent-shaped plastic inserts into the cornea to support the shape, flatten the cone and improve vision.
Cornea transplant: In patients with extreme thinning or corneal scarring, a cornea transplant (keratoplasty) will be needed. Generally, this surgery has a good success rate with proper post operative management and regular follow up.
If you have blurred or distorted vision, schedule your appointment with your nearby eye doctor as soon as possible.
- Cortical cataracts symptoms, causes and treatment - January 7, 2020
- All you wanted to know about Nuclear Cataracts - December 30, 2019
- Cornea: Overview of Corneal Diseases and Common Symptoms - April 30, 2019