Cystoid macular oedema is a painless condition which affects the macula – the central part of the retina (Figure 1.1 and 1.2). This condition occurs when fluid collects in the tissue at the back of the eye, including the area responsible for our central vision. This accumulation of multiple pockets of fluid as cysts in the macular area, is known as cystoid macular oedema.

Figure 1.1. Normal Fundus

Figure 1.2 Cystoid macular oedema
What are the causes
Cystoid macular oedema may commonly be seen following an uncomplicated cataract surgery. A variety of diseases can also lead to this condition including retinal vein occlusion, uveitis (inflammation of the middle coats of the eye), and diabetes. It may less commonly be idiopathic (without any cause) and in cases of retinitis pigmentosa (a genetic condition affecting the photoreceptors).
Symptoms
In CME, the blood vessels in the retina begin to leak or it may also occur when the retinal pigment epithelium is unable to pump the metabolic products out of the retinal tissue. When this occurs, it can cause the macula to swell or thicken. As it is responsible for central or pinpoint vision, macular oedema will cause blurry or distorted vision, affecting the ability to see clearly.
Diagnosis
A thorough dilated fundus examination is necessary for the diagnosis of oedema or swelling of the macular area.
Optical Coherence Tomography, the OCT, shows retinal elevation with multiple cystic spaces within the retinal layers (Figure 2).

Figure 2. OCT scan showing Cystoid Macular Oedema
Treatment
The underlying disease factor causing the macular oedema needs to be addressed. In idiopathic CME or that following uncomplicated cataract surgery, usually, topical NSAIDS may suffice. Topical NSAIDs are also the first line of management in other forms of CME, though most often they’re not sufficient. If there is no proper response seen, posterior subtenon triamcinolone (injection into the outer coat of the eye) may be considered and in resistant cases an Intravitreal triamcinolone/ Ozurdex implant injection may be considered. If the cause of the oedema is vitreous pull on the retina, Vitrectomy with membrane peeling is done to remove the impediment. In case of retinal vein occlusions or in cases of diabetic macular oedema, an anti-VEGF agent may also be tried, especially when a steroid injection may be considered risky, for example, in cases of co-existent glaucoma.
To treat Macular Oedema, the ophthalmologist may need to use medication injection inside the eye (Figure 3). To prepare for it, the eye is cleaned with betadine solution to reduce the chance of infection and then numbed with topical anaesthesia to reduce discomfort during the procedure. The pupils may be dilated or widened with dilating eye drops. The medication is then injected into the vitreous cavity (jelly-like substance occupying the inside of the eye). Pressure may be felt in the eye when the medication is injected.
This injection can reduce swelling of the macula inside the eye. The ophthalmologist is the one who will decide how many injections are needed over a period of time.

Figure 3. Intravitreal injection
Risk Factors
Though very rare, there is risk of possible side effects, which may include but may not be limited to:
- eye pain
- bloodshot eye
- visual disturbances like floaters
- inflammation or swelling of the eye
- retinal detachment
- cataract or clouding of the lens of the eye (in case of steroid injection)
- glaucoma (increased pressure in the eye)
- damage to the retina, cornea or lens
- bleeding
- eye infection
- the need for more treatment including medication or surgery
Though it is extremely rare and we haven’t come across this complication in our practice, it is possible for some people using certain types of medications to have a stroke, haemorrhage or heart attack with injection of anti-VEGF agents. Patients who have had a heart attack or stroke in the last few months need to inform their ophthalmologist about the same and the medications they are using.
Any or all of these complications may decrease vision or possibly even cause blindness and additional procedures may be needed to treat these other complications.
But, then again, Cystoid macular oedema is a vision threatening condition which can be treated effectively (Figure 4). Without treatment, Cystoid Macular Oedema will lead to more vision loss. The main goal in treatment is to get rid of the swelling and better the vision.
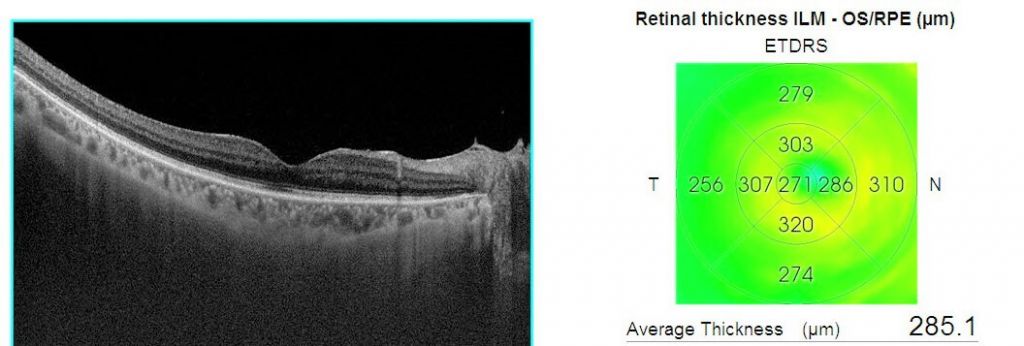
Figure 4. OCT scan of the same patient after treatment
To make an informed decision and for in-depth guidance, visit Neoretina, an NABH Accredited eye care hospital in Hyderabad or you can also log on to https://neoretina.com/ to book a consultation with specialists today.
- Cataract surgery safety during Covid 19 - July 7, 2020
- Exclusive Phaco Pack in Cataract Surgery: Do you need it? - June 9, 2020
- Uveitis treatment in the time of Coronavirus Infection: Dos and Don’ts - March 30, 2020